- Systematic Review
- Open access
- Published:
Effectiveness and cost-effectiveness of community-based mental health services for individuals with severe mental illness in Iran: a systematic review and meta-analysis
BMC Psychiatry volume 24, Article number: 256 (2024)
Abstract
Background
Severe mental illness (SMI) imposes a substantial worldwide burden of disability, highlighting the need for comprehensive and adaptable mental health services. This study aims to assess the efficacy and cost-effectiveness of community-based mental health services (CBMHS) in reducing relapse and rehospitalization rates among individuals with SMI in Iran.
Method
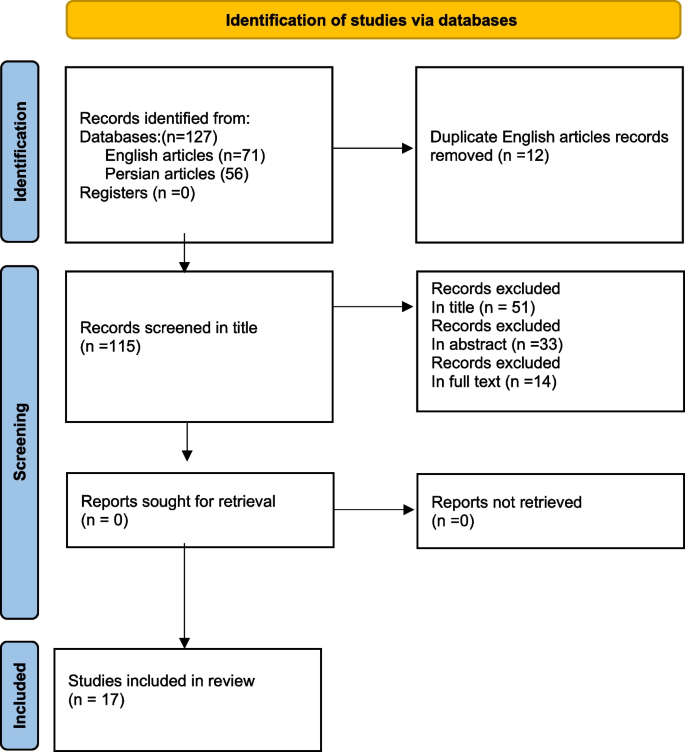
A systematic review and meta-analysis were conducted. Medline, EMBASE, ISI, SCOPUS, and ProQuest were searched until December 2022. We focused on randomized controlled trials, quasi-experimental studies, or economic studies related to individuals with SMI. Out of 127 articles, 17 were selected for a full-text review. The primary outcomes were the severity of psychopathology, rehospitalization rates, and the mental health of caregivers. We also examined community-based interventions and their impact on various outcomes. Data extraction and risk of bias assessment were performed, and critical appraisal was conducted using JBI checklists. Meta-analysis was carried out using STATA software. (PROSPERO registration. CRD42022332660).
Result
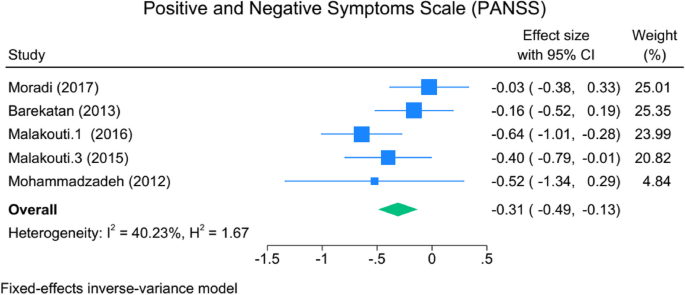
Rehospitalization rates among patients who received CBMHS were significantly lower, with an odds ratio of 2.14 (95% CI: 1.44 to 3.19), indicating a 2.14 times lower likelihood than those who received treatment as usual. A reduction in psychopathology accompanied this, SMD: -0.31, 95% CI: -0.49 to -0.13, I2 = 40.23%). Moreover, there was a notable improvement in social skills (SMD: -0.7, 95% CI: -0.98 to -0.44, I2 = 0.00%). The burden on caregivers also decreased (SMD: -0.55, 95% CI: -0.99 to -0.1, I2 = 63.2). The Incremental Cost-Effectiveness Ratio (ICER) for QUALY was acceptable, albeit with a wide range of 613 to 8400 Dollars.
Conclusion
CBMHS has demonstrated effectiveness and efficiency in Iran as a developing country. Additionally, it shows promise in mitigating the shortage of acute psychiatry beds. Using multiple data collection tools poses a limitation regarding data consolidation and conducting a meta-analysis.
Introduction
Severe mental illness (SMIs) is a prevalent global cause of disability. In 2019, mental disorders contributed to approximately 418 million disability-adjusted life years (DALYS), accounting for 16% of global DALYS. This represents a significant increase compared to previous estimates. The World Health Organization's (WHO) Action Plan (2013–2030) emphasizes establishing inclusive and adaptable community-based mental health and social care services. The goal is to empower individuals affected by these disorders to exercise their full human rights and gain timely access to culturally appropriate, high-quality healthcare and social support. This approach promotes recovery, enables individuals to achieve optimal well-being, actively participate in society and employment, and eliminates stigmatization and discrimination [1].
Although medication is essential for symptom control and relapse prevention, it is insufficient to address the social needs of patients with severe mental illness. In recent years, there has been notable progress in pharmacotherapy, particularly in managing the acute phase of the disorder, which has subsequently increased the inclination toward providing community-based mental health services (CBMHS) [2, 3]. The various aspects of psychiatric disorders, including their health, familial, social, and economic dimensions, also highlight the different CBMHS, such as home visits, outpatient services, community-based rehabilitation, psychological training, family therapy, and other methods. Additionally, it acknowledges the financial burden that SMIs place on families and governments, with an estimated economic impact of approximately USD 5 trillion in 2019 [4].
Based on the findings of the Iranian Mental Health Survey (IranMHS) conducted in 2011, nearly a quarter of the population experiences psychiatric disorders, of which 3 to 5 presents suffer severe illness [5]. Furthermore, it emphasizes that these conditions are the leading cause of disability among individuals aged 10 to 40 in Iran [6].
Studies demonstrate that the provision of CBMHS effectively reduces relapse and rehospitalization rates in patients and alleviates the burden on families. Additionally, by lowering hospitalization and daycare costs, the economic burden associated with SMIS is reduced. However, offering these services in Low- and Middle-Income Countries (LMICS) encounters obstacles related to social, cultural, and financial factors [7]. In Iran, notable attention has been given to providing comprehensive, integrated, and responsive mental health services in community settings [8]. Conducted in Iran, it demonstrated a 67% reduction in hospitalization rates after individuals received CBMHS [9]. There are numerous studies conducted worldwide that have demonstrated the effectiveness and cost–benefit of community-based services [10,11,12,13]. However, in parallel with the expansion of community-based services, long-term hospitalization and asylum-like services were expanded nationwide in the last two decades. Our intention in this study was not to evaluate these services at the global level, but we checked whether this system works in Iran's cultural, social, and economic conditions, and maybe this Rio systematic is useful for mental health policymakers and shows that the development of these services requires It takes more effort. For this reason, we focused on Iranian studies.
To address the knowledge gap, we conducted a systematic review and meta-analysis of Randomized Clinical Trials (RCTs), quasi-experimental studies, or economic studies to evaluate the cost-effectiveness and cost benefit effectiveness of CBMHS in reducing relapse and rehospitalization rates among patients with SMIs. The findings of this study may have implications not only for future research in Iran but also for neighboring countries.
Methods
Eligibility criteria
RCTs, quasi-experimental studies, or economic studies conducted on specific outcomes such as clinical relapse, rehospitalization, cost, and the severity of psychopathology, were included. The intervention on individuals with a diagnosis of psychotic spectrum disorder (schizophrenia, schizophreniform, and other long-lasting psychotic disorders), Bipolar Mood Disorders (BMD), or severe refractory major depression were considered were considerd.
Amongst them, studies with any community-based intervention, including home-visit services (by professionals or peers and family members), telephone follow-up, family psychoeducation, and skill training, and the studies which aim the caregivers' knowledge, burden, and mental conditions as by proxy groups to have an impact on SMI clinical outcome were included.
Rehospitalization, relapses, clinical condition and severity of the symptoms, treatment adherence, economic outcomes including QALYS, CER (Cost-Effectiveness Ratio), social functioning, quality of life, and family knowledge were outcomes of interest.
Exclusion criteria were any studies performed on individuals with substance use disorders, intellectual disability, brain trauma, or; the intervention model was not transparent and did not have a follow-up interval.
The study protocol had been approved by the Ethics Committee of the Iran University of Medical Sciences (code: IR.IUMS.REC.1400.733) and registered in PROSPERO. (CRD42022332660, available here: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022332660.)
Search strategy
We systematically reviewed the published literatures on the intervention models for SMIs in Iran. This review includes all RCTs, quasi-experimental studies, or economic studies reporting on the effectiveness and cost-effectiveness of community-based care and interventions designed to promote social engagement among individuals with SMI.
The search was conducted for articles published in English using databases such as Medline, EMBASE, ISI, SCOPUS, and ProQuest. Additionally, peer-reviewed papers in the Persian language, were accessed via Iranian websites including SID, MAGIRAN, and Iran doc. Our search terms (keywords and Mesh terms) reflected central concepts: severe mental illness, models of intervention, outcome, and relapse. We limited our search to publications in English and Persian available in full text. If the full text was not available, the authors were contacted. publications included in the study were published until December 2022, the complete search strategy can be found in the Supplementary Material 1: Appendix.
Since this study aimed to estimate the effectiveness of CBMHS, and some of the included articles used alternative versions of the questionnaires, we excluded the data from alternative versions. We extracted the relevant data by carefully studying the tables and text.
Screening and data extraction
Two independent reviewers (S.N., M.T.) assessed article titles and abstracts to exclude unrelated records. The full text of the remaining studies was also reviewed independently by S.N. and M.T., with unrelated articles being excluded. Any disagreements were resolved through discussion and judgment by the principal investigator (SK.M.).
A pre-designed data sheet was completed for each of the included studies. Data extraction from each included paper was performed by two independent authors (S.N., M.T.) based on the author's name, publication year, journal name, study population, city of the study population, sex, sample size, type of intervention, and tools.
Risk of bias assessment
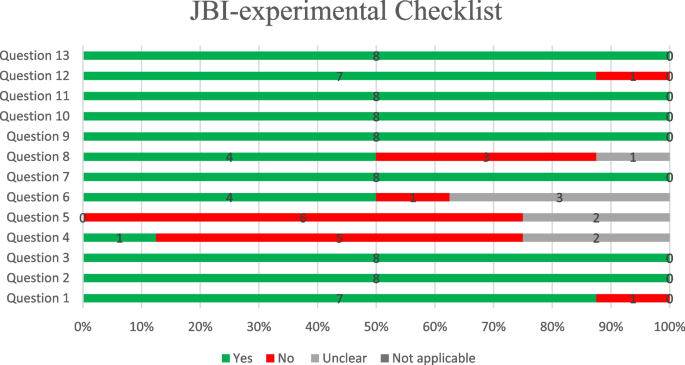
The relevant JBI critical appraisal checklist regarding the study designs (i.e., RCT, quasi-experimental, and economic evaluation) was used to evaluate the articles. JBI critical appraisal Checklist for RCTs has 13 questions evaluating different methodological aspects of an RCT, including randomization, concealed allocation, blinding, follow-up, and analysis (all versions of JBI available: https://jbi.global/critical-appraisal-tools).
Statistical analysis
To ensure comparable results, we calculated Standardized Mean Differences (SMD) and 95% confidence interval between the intervention and control groups [10]. SMDs were calculated, where available, to assess the intervention's effectiveness during the follow-up period (i.e., a pre-post comparison in the experimental group) and to measure the differences between the experimental and control groups at the follow-up time (i.e., calculated as the post–pre-experimental mean minus the post–pre control mean). The odds ratio and 95% confidence interval were calculated to compare the rehospitalization rate between the groups.
The data were analyzed using STATA, version 17.0 (STATA Corporation, College Station, TX, USA). The statistical heterogeneity between the studies was assessed using the I2 statistic, which was able to measure the inconsistency across the results of the studies and describe the proportion of the total variations based on their estimates due to the presence of heterogeneity rather than sampling errors. A random-effects model was used if heterogeneity was observed (the I2 values > 50).
Result
Seventy-one articles were selected through the English-language website, and fifty-six Persian-language articles were selected through the Iranian website. After removing duplicates, 115 articles remained. In the next steps, the titles and abstracts were reviewed, and 84 articles were excluded. The full text of thirty-one articles was reviewed, of which 14 unrelated articles were excluded. Finally, 17 English and Persian articles were included in the study (Fig. 1).
Critical appraisal and risk of bias assessment
The results of the risk of bias and critical appraisal in the qualitative assessment of the articles are as follows. We have 8 experimental articles that meet the inclusion criteria for our study. These articles were selected based on their relevance to our research question and their adherence to our predetermined criteria for experimental design. We evaluated the articles based on the JBI critical appraisal checklist (Fig. 2). Question four (Were participants blind to treatment assignment?) And question five (Were those delivering treatment blind to treatment assignment?) Were not applicable for most of the studies as in the communicate based intervention it is not feasible for the participants and the person who deliver the services to be blind of interventions. The rest of the items were enough qualified to rely on the results (Fig. 2). The result of the quasi experimental and economy studies checklists depicted in the Supplementary Material 1:Appendix.
The demographic characteristics of included articles
Demographic characteristics of included articles revealed Table 1.
The results of intervention comparing before and after 12-months follow-up presented. The findings related to the tools used in intervention studies are presented in Table 2. As noted, most tools reported a weak level of heterogeneity(I2), so the meta-analysis has not been performed. The meta-analysis was conducted for rehospitalization, PANSS (Positive and Negative Syndrome Scale) as a psychopathology assessment tool and KELS (Kohlman Evaluation of Living Skills of the patients) and FEIS variables indicating psychological distress in caregivers.
The rehospitalization rate
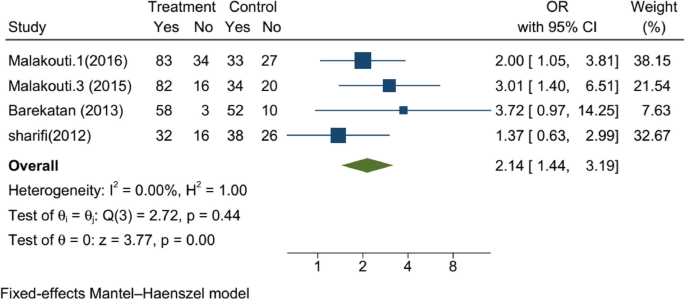
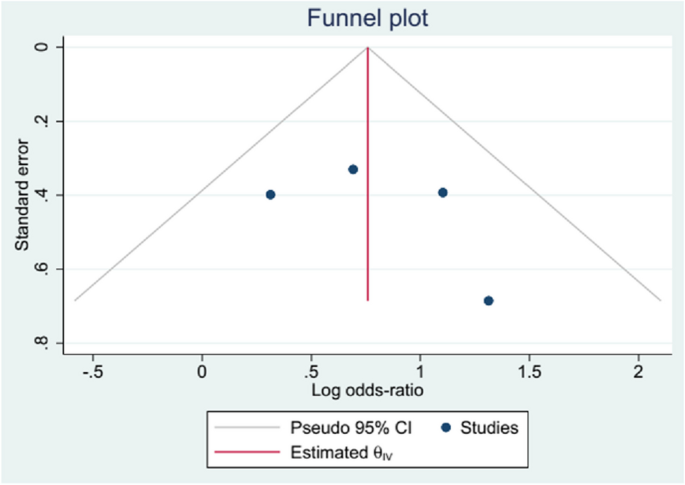
One of the study's primary goals was to evaluate the effect of any CBMHS on rehospitalization after the index discharge. The CBMHS included home-visit and telephone follow-ups, the rehospitalization rate among patients who received CBMHS (with a total of 595 participants in both intervention and control groups) was 2.14 times lower compared to those who received treatment as usual (OR: 2.14,95%CI: 1.44, 3.19). Mohebi [17] was the only article that used Medication Adherence Rating Scale (MARS) to evaluate the compliance of the patient with treatment (SMD: 3.15, CI: 95% 2.31, 3.98). The result of the meta-analysis of rehospitalization among four studies showed in Fig. 3. There was not any publication bias. It shown as Fig. 4.
Severity of psychopathology
Out of 17 studies, 5 used PANSS to evaluate the effect of intervention on psychopathology, whose data were amenable to analysis (with a total of 669 participants in both intervention and control groups). Meta-analysis shows that after 12 months of intervention, CBMHS are successful in reducing significantly of the severity of psychopathology (SMD: -0.31, 95%CI: -0.49 to -0.13, I2 = 40.23%). Akbari [18] was the only one that used ANSQ -Anderson Negative Symptoms- (SMD: -0.581, 95%CI: -1.312, 0.149). The meta-analysis of the studies for PANSS showed in Fig. 5.
The result of meta-analysis on the YOUNG (evaluating the severity of Bipolar mood disorder) shows significant difference by implementing the intervention (SMD: -0.764, 95% CI: -1.274, -0.253, I2 = 85.22%), however the heterogeneity among four studies were not acceptable.
Upon visual examination of the funnel plot, no significant signs of asymmetry were observed (located in the Supplementary Material 1: Appendix).
Social skills as secondary outcomes of the study could be considered as one of the outcomes of any intervention that aims to help the patient to be as independent as possible in the family and society. Just two studies used KELS to evaluate the social skills of the patients. The result of KELS shows a high effect size (SMD: -0.7, 95%CI: -0.98 to -0.44, I2 = 0.00%), and the community-based interventions are more promising. The same result was revealed by the study of Shahmiri (2014) by Matson evaluation of social skills (MESS) (SMD: -0.877, 95%CI: -1.749, 0.041) (lower scores indicating better functioning).
The tools of ACIS Assessment of Communication and Interaction Skills (mean difference 1.747 (CI: 1.08, 2.41).) Higher scores indicate better skills, such as DSK Dehbozorgi's social skills (SMD: 0.835, 95%CI: 0.088, 1.581). (Lower scores indicate lower social skills).
The burden of the caregivers was evaluated by FEIS (evaluating the burden of the caregivers) in the meta-analysis (not shown in the article). It shows that again in the two articles, the effect size was -0.55 (SMD: -0.55, 95%CI: -0.99, -0.1, I2 = 63.2) (in favor of community-based services.
For the CSQ, which evaluated the satisfaction of the clients from the services, there were not any significant differences with the control group. In the study of Sharifi [14], the quality of life of (WHOQOL) patients has been improved marginally (SMD:-0.246, 95%CI: -0.500, 0.007) (P = 0.057). However, in the study of Hojati- Abad [27] WQOLCQ (Wisconsin Quality of Life Client Questionnaire (SMD: 0.798, 95%CI: 0.29, 5, 1.301), there was not any significant difference.
Economic evaluation studies
For economic evaluation we considered tow indexes reported incremental cost-effectiveness ratios (ICER) [28] and Quality-Adjusted Life Year (QUALY) [29, 30], which is are more common indexes economic evaluation.
The QALY serves as a metric for assessing the worth of health outcomes. As health is contingent upon both lifespan and well-being, the QALY was formulated as an endeavor to amalgamate the value of these attributes into a solitary index. In the field of mental health, improving the quality of life for patients and reducing the burden of the disease not only for the patients themselves but also for their families and society as a whole. QALYs can be integrated with medical expenses to derive a final universal measure of cost/QALY. This parameter facilitates the comparison of the cost-effectiveness of various treatments without bias.
In numerous healthcare systems, determinations regarding the reimbursement and availability of new medications hinge upon health technology assessments. These assessments, involve the evaluation of an ICER. Decision-makers then weigh the ICER against a predetermined benchmark for cost-effectiveness, referred to as the cost-effectiveness threshold (CET), in order to ascertain whether reimbursement should be granted or withheld [28].
We identified two reports that met our inclusion criteria concerning economic evaluations of community-based interventions to improve the mental health of individuals with SMI [13, 21]. In both studies were included QUALY and ICER.
Malakouti et al. ICER for aftercare home services following the discharge of individuals with SMI. Their analysis was based on a 12-month follow-up of participants in a clinical trial conducted between 2007 and 2008. They found that the ICER was 5.7 million Rials (IRR) per QALY when using general practitioners (GPs) as care providers during home visits and 5.0 million IRR per QALY when replacing GPs with nurses [13]. In a separate study, Moradi-Lakeh et al. conducted a cost-utility analysis of aftercare services following the discharge of individuals hospitalized for SMI. Their analysis was based on a clinical trial performed from 2012 to 2014, with a 20-month follow-up. They reported an ICER of US$8,399 (95% CI: 8,178–8,620) per QALY for the intervention [13]. It is worth noting that the services provided by the second study were more comprehensive. In these two studies showed that community-based interventions can be useful in terms of cost–benefit and cost-effectiveness.
While the ICER measures in these two studies differed considerably (partly due to a significant fluctuation in IRR-USD exchange rates $1 = 935 to 10,402 IRR, and other services provided by the second study included the expenses of general psychologists, supervising psychiatrists, as well as the costs of weekly co-ordination meetings of home visit teams, costs of classes for caregivers' education, training of social skills), both were found to be below the World Health Organization's recommended threshold for cost-effectiveness of health interventions [13, 21]. The second study aimed to provide the cheapest and most effective intervention and evaluated the feasibility of providing such CBMHS. However, from $ 613 to $8400, it is feasible to provide such services while considering the exchange and inflation rates.
Discussion
Out of 127 English and Persian language articles which were conducted in IRAN, seventeen met the eligibility criteria for inclusion in the systematic review and meta-analysis. community-based services effectively reduced rehospitalizations by 2times. reduction in psychopathology with moderate effect sizes. economic cost-effectiveness, with ICER values falling below the recommendations set by the WHO s.
Community psychiatry was launched in the USA in 1970 [31], community psychiatry was launched in the USA in 1970 [31] Reducing hospitalization, enabling individuals to have an active social life in society [32], and providing holistic care are among the main goals of community psychiatry community psychiatry was launched in the USA in 1970 [31].
CBMHS, including home visits, telephone follow-ups, case management systems, intensive care systems, and other CBMHS developed in different societies, have emerged and expanded to address this new challenge [32]. Even in a crisis, CBMHS mobile crisis intervention can reduce the number of readmissions [33]. Providing and connecting discharged patients to community services as soon as possible is a critical issue to prevent readmission [34].
On the other hand, the evidence shows that the direct daily costs for community-based social psychiatric care were about half the costs of inpatient treatment over the entire period [34, 35]. However, reducing the number of readmissions depends on the intensity of community services, and it may yield different results in some societies [36].
Some reasons may be nominated for reduction of rehospitalization [37, 38]. However, compared with the developed societies, we need to examine this issue from a dual perspective. First, in addition to having social activities and supporting the patients to have an almost independent life, second, the shortage of psychiatric beds is an essential matter in our country's mental health services. According to the according recommended assesment, we should have forty more than 56 thousand psychiatric beds in Iran [39, 40] which falls behindrrrr. With the best estimation, we have thirty thousand psychiatric beds, of which fifty percent belong to the Welfare Organization for long-term hospitalization and rehabilitation [40]. Therefore, an extension of CBMHS psychiatry could help the patient and their family but also help the national mental health service to compensate for the shortage of facilities. Exacerbating the severity of psychopathology could increase the odd behaviors and tension in the family, leading to the patient's hospitalization [41, 42]. Reducing the severity of psychopathology, as revealed in the study results as the severity of PANSS and YMRS in the current study, could be helpful. Increasing adherence to medication due to frequent contact (in person or by telephone) encourages the patient to comply with the treatment, which is the main reason for reducing the severity of psychopathology.
Having a long-duration mental health stability state without exacerbation of the symptoms, in addition to psychoeducation and behavioral rehearsal, which is part of community-based intervention, could provide suitable opportunities for the patient to retrieve his/her behavioral skills or learn new skills, which are necessary for independent living [43, 44]. Social skills, evaluated by KELS and MESS, showed promising outcomes for CBMHS with remarkable effect size. However, gaining social skills requires intense and close supervision, which any community-based intervention may not obtain, as shown by the study of Jamshidi [25]; the results of this study are controversial ACIS.
The burden and mental health of the caregivers for chronic diseases such as schizophrenia, bipolar mood disorder, and dementia are essential in mental health services. Given that in developing countries [45, 46], taking care of patients is on the shoulders of the families, providing aftercare services and regular contact with the patient and the caregivers could help them overcome the long-lasting problems in their family. The reduction of burden and improvement of the mental health condition of the caregivers show that such services have a positive impact on them [44].
Satisfaction with the services and quality of life, which did not exhibit significant differences from the control group in our study, remains a topic of extensive debate. Satisfaction and quality of life depend on physical and mental health and suitable living conditions such as housing, jobs, and income, which are not fulfilled by community-based services and are beyond the scope of these services and require intersectoral collaboration [12, 21, 38].
The challenge of the studies performed in Iran as CBMHS was using multiple tools with similar goals to evaluate corresponding variables. This hinders the ability to compare and analyze the results effectively. For instance, the study employed four different tools to measure life skills. Also, despite the history of CBMHS in Iran, there is a lower publication rate for the results of these interventions and programs. The expectation of having more articles that evaluate this specific area emphasizes the need for attention to be given to this issue.
Conclusion
The findings of community-based studies in Iran, although rare, showed that in line with international studies, this type of service is compatible and effective in Iran's economic, social, and cultural conditions. Even though there are challenges regarding patient satisfaction and organizational interdepartmental cooperation. These findings emphasize that community-based services not only in Iran but also in similar countries should be preferred over long-term inpatient services.
Availability of data and materials
This is an evidence synthesis study, all data is available from the primary research studies, or can be circulated from the corresponding author.
References
Singh OP. Comprehensive mental health action plan 2013–2030: we must rise to the challenge. Indian J Psychiatry. 2021;63:5415–7.
Ojha SP, Pant SB. Community based rehabilitation for task shifting in mental health. J Psychosoc Rehabil Ment Health. 2018;5:109–10.
Keegan J. Community-based mental health care: bridging the gap between community care and primary care. Aust N Z J Ment Health Nurs. 1998;7(3):95–102.
Arias D, Saxena S, Verguet S. Quantifying the global burden of mental disorders and their economic value. EClinicalMedicine. 2022;54.
Sharifi V, Amin-Esmaeili M, Hajebi A, Motevalian A, Radgoodarzi R, Hefazi M, et al. Twelve-month prevalence and correlates of psychiatric disorders in Iran: the Iranian Mental Health Survey, 2011. Arch Iran Med. 2015;18(2):76–84.
Forouzanfar MH, Sepanlou SG, Shahraz S, Dicker D, Naghavi P, Pourmalek F, et al. Evaluating causes of death and morbidity in Iran, global burden of diseases, injuries, and risk factors study 2010. Arch Iran Med. 2014;17(5):304–20.
Rathod S, Pinninti N, Irfan M, Gorczynski P, Rathod P, Gega L, et al. Mental health service provision in low-and middle-income countries. Health Serv Insights. 2017;10:1178632917694350.
Sharifi V, Abolhasani F, Farhoudian A, Amin-Esmaeili M. Community mental health centers in Iran: planning evidence-based services. Iran J Psychiatry Clin Psychol. 2014;19(3):163–76.
Malakouti SK, Nojomi M, Panaghi L, Chimeh N, Mottaghipour Y, Joghatai MT, et al. Case-management for patients with schizophrenia in Iran: a comparative study of the clinical outcomes of mental health workers and consumers’ family members as case managers. Community Ment Health J. 2009;45:447–52.
Andrade C. Mean difference, Standardized Mean Difference (SMD), and their use in meta-analysis: as simple as it gets. J Clin Psychiatry. 2020 2020/09//; 81(5):[20f13681 p.]. Available from: http://europepmc.org/abstract/MED/32965803.https://www.psychiatrist.com/read-pdf/11349. https://0-doi-org.brum.beds.ac.uk/10.4088/JCP.20f13681.
Barekatain M, Maracy MR, Rajabi F, Baratian H. Aftercare services for patients with severe mental disorder: a randomized controlled trial. J Res Med Sci. 2014;19(3):240–5.
Malakouti SK, Nojomi M, Mirabzadeh A, Mottaghipour Y, Zahiroddin A, Kangrani HM. A comparative study of nurses as case manager and telephone follow-up on clinical outcomes of patients with severe mental illness. Iran J Med Sci. 2016;41(1):19–27.
Moradi-Lakeh M, Yaghoubi M, Hajebi A, Malakouti SK, Vasfi MG. Cost-effectiveness of aftercare services for people with severe mental disorders: an analysis parallel to a randomised controlled clinical trial in Iran. Health Soc Care Community. 2017;25(3):1151–9.
Sharifi V, Tehranidoost M, Yunesian M, Amini H, Mohammadi M, Jalali RM. Effectiveness of a low-intensity home-based aftercare for patients with severe mental disorders: a 12-month randomized controlled study. Community Ment Health J. 2012;48(6):766–70.
Babokani ZS, Ghazanfari A, Ahmadhi R, Chorami M. The comparison of the effectiveness of behavioral activation and psychosocial on mental cognitive functions in women with chronic schizophrenia. Q J Psychol Stud. 2020;15(4):91–108.
Malakouti SK, Chimeh N, Panaghi L, AhmadAbadi Z, Nojomi M. The effectiness of two case management methods on mental health, knowledge, and burden of schizophernics. Family Member Fam Res. 2009;5(17):29–42.
Mohebi P, Fallahi-Khoshknab M, Rahgoi A, Tabrizi K, Khodaei-Ardakani M-R. Effect of the community re-entry program on medication adherence in patients with bipolar disorder type I. Iran J Rehabil Res Nurs. 2017;3:58–65.
Akbari M, Saeidi S. The effectiveness of psychosocial rehabilitation in reducing negative symptoms and improving social skills of chronic schizophrenia patients. Shenakht J Psychol Psychiatry. 2017;4(3):21–35.
Fayyazi Bordbar MR, Soltanifar A, Talaei A. Short-term family-focused psycho-educational program for bipolar mood disorder in Mashhad. Iran J Med Sci. 2009;34.
Ahmadi A, Farahbakhsh K, Moatamedy A, Khodaei M, Safi MH. The effectiveness of family psychological training on prevention of recurrence of symptoms in patients with schizophrenia spectrum disorders. Iran J Psychiatr Nurs. 2020;8(3):93–103.
Malakouti SK, Mirabzadeh A, Nojomi M, Ahmadi Tonkaboni A, Nadarkhani F, Mirzaie M, et al. Clinical outcomes and cost effectiveness of two aftercare models provided by general physicians and nurses to patients with severe mental illness. Med J Islam Repub Iran. 2015;29:196.
Shahmir E, Talebizadeh M, Jafarifard S. The effectiveness of the returning to society program in improving the social skills of schizophrenic patients. Thoughts Behav Clin Psychol. 2014;9(31):27–36.
Mohammadzadeh Nanehkaran S, Karbalaie Noori A, Hosseini SA. Effect of Community Re-entry Program (CRM) in patients with schizophrenia. Arch Rehabil. 2013;14(2):22–8.
Fallahi-Khoshknab M. Effectiveness of Psychiatric Nursing Home Care Services for Psychiatric Status in Schizophrenics. Arch Rehabil. 2007;8:77–81.
Jamshidi F, Shayan A, Forouhari S, Taherkhani H, Seyedi M. The effect of community Re-entry program (CRP) on social function of patients with chronic mental disorders. Acta Med Mediterr. 2016;32(Specia):1311–6.
Dashtbozorgi B, Ghadirian F, Khajeddin N, Karatni K. Effect of family psychoeducation on the level of adaptation and improvement of patients with mood disorders. Iran J Psychiatry Clin Psychol. 2009;15(2):193–200.
Hojjati-Abed E, Karbalaaei-nouri A, Rafiei H, Karimlou M. The efficacy of psychosocial occupational therapy services on quality of life of chronic pschiatric patents. Arch Rehabil. 2010;11(1):0.
Berdud M, Ferraro J, Towse A. A theory on ICER pricing and optimal levels of cost-effectiveness thresholds: a bargaining approach. Front Health Serv. 2023;3:1055471.
Prieto L, Sacristán JA. Problems and solutions in calculating quality-adjusted life years (QALYs). Health Qual Life Outcomes. 2003;1:80.
Rand LZ, Kesselheim AS. Controversy over using quality-adjusted life-years in cost-effectiveness analyses: a systematic literature Review. Health Aff (Millwood). 2021;40(9):1402–10.
Dean C, Phillips J, Gadd E, Joseph M, England S. Comparison of community based service with hospital based service for people with acute, severe psychiatric illness. Br Med J. 1993;307(6902):473–6.
Kisely S, Yu D, Maehashi S, Siskind D. A systematic review and meta-analysis of predictors and outcomes of community treatment orders in Australia and New Zealand. Aust N Z J Psychiatry. 2021;55(7):650–65.
Guo S, Biegel DE, Johnsen JA, Dyches H. Assessing the impact of community-based mobile crisis services on preventing hospitalization. Psychiatr Serv. 2001;52(2):223–8.
Haywood TW, Kravitz HM, Grossman LS, Cavanaugh JL, Davis JM, Lewis DA. Predicting the" revolving door" phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. Am J Psychiatry. 1995.
Bachrach LL. Deinstitutionalisation: promises, problems and prospects. Ment Health Serv Eval. 1996:3–18.
Sytema S, Burgess P, Tansella M. Does community care decrease length of stay and risk of rehospitalization in new patients with schizophrenia disorders? A comparative case register study in Groningen, The Netherlands; Victoria, Australia; and South-Verona. Italy Schizophr Bull. 2002;28(2):273–81.
Joynt KE, Sarma N, Epstein AM, Jha AK, Weissman JS. Challenges in reducing readmissions: lessons from leadership and frontline personnel at eight minority-serving hospitals. Jt Comm J Qual Patient Saf. 2014;40(10):435–7.
Phillips MS, Steelesmith DL, Campo JV, Pradhan T, Fontanella CA. Factors associated with multiple psychiatric readmissions for youth with mood disorders. J Am Acad Child Adolesc Psychiatry. 2020;59(5):619–31.
Allison S, Bastiampillai T, Licinio J, Fuller DA, Bidargaddi N, Sharfstein SS. When should governments increase the supply of psychiatric beds? Mol Psychiatry. 2018;23(4):796–800.
Malakouti SK, Keshavarz Akhlaghi A, Shirzad F, Rashedi V, Khlafbeigi M, Moradi Lakeh M, et al. Urban mental health initiative: developing interdisciplinary collaboration, the role of the family physician in management of severe mentally ill patients. Iran J Psychiatry Clin Psychol. 2021;27(1):104–19.
Hinojosa-Marqués L, Domínguez-Martínez T, Barrantes-Vidal N. Family environmental factors in at-risk mental states for psychosis. Clini Psychol Psychother. 2022;29(2):424–54.
Kuhney FS, Miklowitz DJ, Schiffman J, Mittal VA. Family-based psychosocial interventions for severe mental illness: social barriers and policy implications. Policy Insights Behav Brain Sci. 2023;10(1):59–67.
de Pablo GS, De Micheli A, Nieman DH, Correll CU, Kessing LV, Pfennig A, et al. Universal and selective interventions to promote good mental health in young people: systematic review and meta-analysis. Eur Neuropsychopharmacol. 2020;41:28–39.
Estrada-Fernández ME, Gil-Lacruz M, Gil-Lacruz AI, Viñas-López A. The impact of community care: burden and quality of life of the informal caregivers of patients with severe mental disorder. J Community Psychol. 2022;50(1):487–501.
Ofovwe CE, Osasona SO. Burden of caregiving among caregivers of patients with severe mental illnesses in Benin City. Nigeria Afr Health Sci. 2022;22(2):657–67.
Ahmadzadeh Asl M, Shojaee A, Shariati B, Rasoolian M, Rashedi V. A comparative study on the burden of disease of schizophrenia, bipolar disorder type I, and autism spectrum disorder on the family caregivers in Iran. Arch Rehabil. 2021;22(3):320–41.
Acknowledgements
Not applicable.
Funding
The current study has been financially supported by the Iran University of Medical Sciences (Registration number: IR.IUMS.REC. 1400–1-99–21128). The funders had no role in the study implementation, data collection and analysis, or interpretation of study results.
Author information
Authors and Affiliations
Contributions
Conceived the project (SKM); Developed the protocol (SKM, SN, KT, MT); Carried out the searches (SN, MT, KT), carried out the synthesis (MT, SN), Interpreted the findings (SKM, MT, KT), drafted the manuscript (SKM, MT), approved the manuscript (SKM). SKM is the guarantor of this review. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol had been approved by the Ethics Committee of the Iran University of Medical Sciences (code: IR.IUMS.REC.1400.733) and about consent and participate: Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Taban, M., Nooraeen, S., Tanha, K. et al. Effectiveness and cost-effectiveness of community-based mental health services for individuals with severe mental illness in Iran: a systematic review and meta-analysis. BMC Psychiatry 24, 256 (2024). https://0-doi-org.brum.beds.ac.uk/10.1186/s12888-024-05666-7
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/s12888-024-05666-7